Clear CVD Benefit With Bempedoic Acid: CLEAR Outcomes
The FDA required a CV outcomes trial to show the already-approved drug reduced the risk of MACE. The results are in.
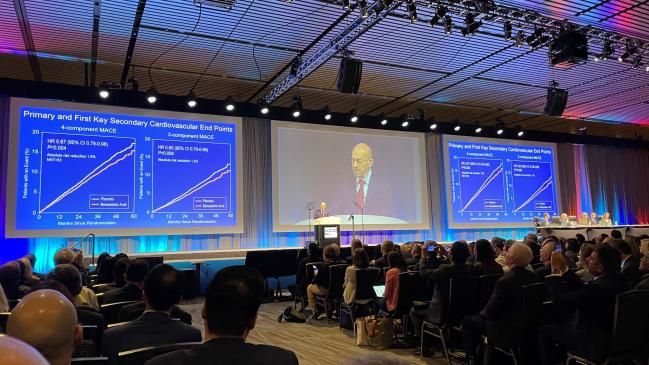
NEW ORLEANS, LA—(UPDATED) Treating high-risk patients who are unable to tolerate statin therapy with bempedoic acid (Nexletol; Esperion) lowers the risk of major adverse cardiovascular events, according to results of the eagerly anticipated CLEAR Outcomes trial.
Among patients who couldn’t take a statin because of unacceptable side effects, the use of bempedoic acid reduced the relative risk of the primary endpoint of death from cardiovascular causes, nonfatal MI, nonfatal stroke, or coronary revascularization by 13% compared with placebo (HR 0.87; 95% CI 0.79-0.96). The reduction in risk was driven by a 23% lower risk of fatal or nonfatal MI and a 19% lower risk of coronary revascularization.
“This is a controversial topic,” Steven Nissen, MD (Cleveland Clinic, OH), chair of the CLEAR Outcomes executive committee, told TCTMD. “There are people who don’t think that statin intolerance exists—I personally think they’re wrong—but I sit in the clinic and these people walk in and they’ve had a couple of myocardial infarctions, bypass surgery, or seven stents, and their LDL-cholesterol levels are high. They will look at me in the eye and say, ‘I can’t take a statin—whenever I start any statin, my muscles hurt.’ We really have not had a go-to therapy for these people.”
Nissen, who kicked off the late-breaking science session at the American College of Cardiology/World Congress of Cardiology (ACC/WCC) 2023 meeting, characterized the reduction in MACE with bempedoic acid as a “moderate” benefit, but stressed the drug will plug a gap in care. There was no reduction in mortality with bempedoic acid, but Nissen said that finding was expected, noting there was no reduction in death with the powerful PCSK9 inhibitor evolocumab (Repatha; Amgen) in FOURIER. There was a 15% relative reduction in all-cause mortality with alirocumab (Praluent; Sanofi/Regeneron) in the higher-risk ODYSSEY Outcomes population.
“The bottom line is we can’t tell people these drugs will reduce their risk of death in the short run,” he said. “We can tell them it does reduce their risk of cardiovascular morbidity.”
Seth Martin, MD (Johns Hopkins Medicine, Baltimore, MD), who wasn’t involved in CLEAR Outcomes, called it a “win” for bempedoic acid. He was pleased to see the benefit extend across both the primary- and secondary-prevention parts of the trial, noting that everybody in the study had relatively high baseline LDL-cholesterol levels, which reflects their inability to tolerate statin therapy. Additionally, follow-up at 3.4 years was longer than the PCSK9 inhibitor outcomes trials, which ran for approximately 2 years, but was shorter than IMPROVE-IT with ezetimibe.
“Considering those factors, it does look like the amount of risk reduction with MACE was what we would expect from the amount of LDL-cholesterol reduction,” Martin told TCTMD. “That’s a big win. It’s really quite remarkable that this relationship between LDL-cholesterol levels with cardiovascular risk has stood the test of time with multiple nonstatin drugs, in addition to the statin class. It’s remarkable that the absolute amount of LDL cholesterol-lowering—not necessarily the percentage amount—has been linked so clearly to cardiovascular outcome benefits. It was nice to see that relationship reinforced once again.”
CLEAR Outcomes was published simultaneously in the New England Journal of Medicine.
Prevalence of Statin Intolerance Ranges
The US clinical cholesterol guidelines recommend high-intensity statin therapy for patients with atherosclerotic cardiovascular disease (ASCVD) and those at high risk for ASCVD. The recent years have seen a number of other lipid-lowering agents come to market, including PCSK9 inhibitors and inclisiran (Leqvio; Novartis), but statins remain the cornerstone of primary and secondary prevention.
The prevalence of statin intolerance owing to muscle symptoms ranges across clinical studies, with the number dependent on the definition and patient population. In one analysis, researchers found that 9.1% of patients had statin intolerance as determined by recognized international definitions, while a meta-analysis by the Cholesterol Treatment Trialists’ collaboration published last year found that statin therapy was associated with only a small risk of muscle symptoms. In cohort studies, however, the prevalence of statin intolerance is notably higher, often close to 30% of patients.
Bempedoic acid is an ATP citrate lyase inhibitor that targets the production of cholesterol upstream of the enzyme inhibited by statins. It is similar to a statin, however, in that it reduces hepatic cholesterol synthesis and raises LDL receptor expression, which helps clear LDL cholesterol from circulation. The drug is approved by both the US Food and Drug Administration and the European Medicines Agency as an adjunct to diet and lifestyle changes for lowering LDL cholesterol.
With CLEAR Outcomes, investigators wanted to determine if lowering LDL cholesterol with the drug also lowered major adverse cardiovascular events. The trial included 13,970 primary- and secondary-prevention patients (mean age 65.5 years; 48.2% female) deemed intolerant to statins, which was defined as being unable or unwilling to take statins because of muscle-related adverse effects that began when treatment was started and resolved when stopped. Moreover, all patients had to provide written confirmation that they were intolerant and acknowledge the benefits of statins.
“They had to sign that really scary statement—‘I can’t tolerate these medications called statins even though I know they would reduce my risk of heart attack or stroke or death,’” said Nissen. “So, these are people that definitely wouldn’t take a statin. We thought we needed to do this for ethical reasons. I think we were pretty rigorous about it.”
CLEAR Outcomes: Efficacy Endpoints
|
|
Bempedoic Acid (n = 6,992) |
Placebo (n = 6,978) |
HR (95% CI) |
|
Primary Endpoint |
|||
|
CV Death, Nonfatal MI, Nonfatal Stroke, or Coronary Revascularization |
11.7% |
13.3% |
0.87 (0.79-0.96) |
|
Secondary Endpoints |
|||
|
CV Death, Nonfatal MI, or Nonfatal Stroke |
8.2% |
9.5% |
0.85 (0.76-0.96) |
|
Fatal or Nonfatal MI |
3.7% |
4.8% |
0.77 (0.66-0.91) |
|
Coronary Revascularization |
6.2% |
7.6% |
0.81 (0.72-0.92) |
|
Fatal or Nonfatal Stroke |
1.9% |
2.3% |
0.85 (0.67-1.07) |
|
CV Death |
3.8% |
3.7% |
1.04 (0.88-1.24) |
|
All-Cause Death |
6.2% |
6.0% |
1.03 (0.90-1.18) |
Baseline LDL-cholesterol levels in both treatment arms were 139.0 mg/dL, with 22.7% taking any statin and 11.5% taking ezetimibe prior to randomization. After 6 months, LDL-cholesterol levels were reduced to 107.0 mg/dL with bempedoic acid while LDL cholesterol declined to 136.0 mg/dL in the placebo arm. This translated into a difference of 29.2 mg/dL. C-reactive protein (CRP) levels also declined with bempedoic acid, down 22.6% at 6 months compared with a 2.4% increase in the placebo group.
Over a median follow-up of 40.6 months, treatment reduced the absolute risk of the primary four-component MACE endpoint by 1.6% compared with placebo, a statistically significant difference. The three-component MACE endpoint—CV death, nonfatal MI, or nonfatal stroke—was also significantly reduced with bempedoic acid. Among the 30% of patients without preexisting ASCVD—the primary-prevention group—the relative reduction in MACE was slightly larger than that seen in the secondary-prevention patients.
Bempedoic was generally well tolerated, with no difference compared with placebo in the percentage of patients discontinuing therapy due to adverse events. There was no risk of new-onset diabetes and no difference in reported myalgias, but bempedoic acid was associated with a higher incidence of gout, cholelithiasis, and laboratory elevations of creatinine, uric acid, and hepatic enzyme levels.
There had been some concerns about the risks of tendinitis or tendon rupture with bempedoic acid—the FDA label does advise patients to stop treatment if they experience joint pain, swelling or inflammation, and to rest at the first sign of tendonitis or tendon rupture—but no safety signal emerged in CLEAR Outcomes.
Primary vs Secondary Prevention
Eugene Yang, MD (University of Washington, Bellevue), who spoke with the media during a press conference for the late-breaking clinical trials, said physicians frequently struggle with patients who come to clinic armed with information about the perils of statin therapy. For the high-risk or ASCVD patient who is unable to take statin therapy because of muscle symptoms, bempedoic acid provides an additional option, particularly for those who don’t want to inject a PCSK9 inhibitor.
Yang, chair of the American College of Cardiology’s Prevention of Cardiovascular Disease Council, praised the researchers for including nearly 50% women in the trial, but noted that the study was made up primarily of white participants (91%), limiting the confidence clinicians can have in other groups. “Are we going to be able to really say with confidence that those populations—Asian people and Black people, in particular—with higher cardiovascular mortality will benefit from this drug? I don’t think we can say that. We don’t have enough data,” he commented. Regarding the larger benefit in the primary-prevention patients—there was a 32% reduction in MACE in this group versus a 9% reduction in the secondary-prevention patients—Yang thinks this might come down to the influence of other disease-modifying therapies, such as statins or ezetimibe.
To TCTMD, Michelle O’Donoghue, MD (Brigham and Women’s Hospital, Boston, MA), raised the same issue, wondering why primary-prevention patients had a larger benefit with bempedoic acid than those with established ASCVD. For that reason, a deeper look into the possible differential treatments between the two groups is warranted.
O’Donoghue agreed that statin intolerance remains a contentious debate, but said regardless of whether a patient can’t or won’t take the drugs, they require some type of treatment because of their high baseline risk. “We know that adherence to statin therapy is often not good, and that the frequency of people reporting muscle-related symptom effects is quite common,” she said. “To that end, it’s an important population to study.”
Overall, O’Donoghue said the results are compelling, adding that event curves began to diverge early. Still, “it wasn’t a complete free pass” with bempedoic acid given the higher incidence of gout, cholelithiasis, and renal events. She added that it’s also unknown if bempedoic acid would reduce cardiovascular events in patients on a background of intensive statin therapy or other lipid-lowering therapies.
“You would expect that you’d still see a reduction in clinical events proportional to the amount of LDL reduction observed, but this was not studied,” said O’Donoghue.
Implementing Bempedoic in Clinical Practice
Nissen said they studied bempedoic acid as monotherapy because that was required by the FDA to show it could reduce morbidity and mortality. However, it is also available in a fixed-dose combination with ezetimibe (Nexlizet; Esperion Therapeutics), and when the two agents are used together, the result is on par with what would be expected from a moderate-intensity statin, he said. For this reason, he believes bempedoic acid is most effective when combined with ezetimibe.
“That combination results in a 35% to 40% reduction in LDL cholesterol,” said Nissen. “The problem is without outcomes data in the current era, prescribers won’t prescribe these drugs and payers won’t pay for them. We needed to do this study and we hung in there from 2016 until now and we got an answer that I think is pretty robust.”
Like Nissen, Martin said that while CLEAR Outcomes provided a definitive result, LDL-cholesterol levels were still north of 100 mg/dL after treatment. The US guidelines recommend physicians intensify lipid-lowering therapy with either ezetimibe or a PCSK9 inhibitor if LDL-cholesterol levels are higher than 70 mg/dL in patients with ASCVD (or higher than 100 mg/dL in those with primary hypercholesterolemia).
“The LDL levels were not optimal, even after the intervention,” said Martin, adding that physicians should really be striving for combination therapy.
Additionally, Martin praised the CLEAR Outcomes’ investigators for their informed consent process. One concern, he said, is that clinicians take the positive study results and move on from statins too quickly. “It was very carefully done to engage patients,” he said. “In day-to-day practice, we would just call it shared decision-making, but we need to make sure that we mimic [the informed consent process] in the real world if we are going to move beyond statins. We need to make sure the well-documented benefits and safety of statins have been articulated before going to bempedoic acid.”
Yang agreed. “We have to be very vigilant about reminding ourselves and our colleagues that we have to be aggressive with statin therapy,” he told TCTMD, adding there are data in secondary-prevention patients showing that almost 50% aren’t taking statins. “We’re already doing a very poor job,” he said. Yang added, like Nissen, that he will try five or six different statins before giving up in patients reporting muscle-related symptoms.
In an NEJM editorial, John Alexander, MD (Duke Clinical Research Institute, Durham, NC), says the compelling results should increase the use of bempedoic acid in ASCVD patients and high-risk primary-prevention patients unable or unwilling to take statin therapy. Like the others, Alexander stresses that CLEAR Outcomes should not be interpreted as a green light to bypass statins.
“It is premature, however, to consider bempedoic acid as an alternative to statins,” writes Alexander. “Given the overwhelming evidence of the vascular benefits of statins, clinicians should continue their efforts to prescribe them at the maximum tolerated doses for appropriate patients, including those who may have discontinued statins because of presumed side effects.”
To TCTMD, Martin said one of the biggest issues going forward now is implementation.
“It’s great to have another tool in the tool kit to lower LDL cholesterol and cardiovascular risk, but on a national level there’s been a lack of movement on risk factor control,” he said. “We’ve had new innovation after new innovation, but how do we redesign our healthcare system to get patients optimally treated? That’s part of a larger conversation.”
Yang said the cost of treatment will be a key issue in getting the drug to eligible patients. While cheaper than PCSK9 inhibitors, bempedoic acid remains considerably more expensive than generic statins and ezetimibe. “How are we going to afford an expensive medication like this,” asked Yang. “This is something we’re going to have to think about. It’s not going to be inexpensive. That’s frankly the most important [issue] in how it fits into our armamentarium.”
Michael O’Riordan is the Managing Editor for TCTMD. He completed his undergraduate degrees at Queen’s University in Kingston, ON, and…
Read Full BioSources
Nissen SE, Lincoff AM, Brennan D, et al. Bempedoic acid and cardiovascular outcomes in statin-intolerant patients. N Engl J Med. 2023;Epub ahead of print.
Alexander JH. Benefits of bempedoic acid—clearer now. N Engl J Med. 2023;Epub ahead of print.
Disclosures
- Nissen reports research grants/contracts through C5 Research from AbbVie, AstraZeneca, Bristol-Myers Squibb, Eli Lilly, Esperion Therapeutics, Novartis, and Silence Pharmaceuticals. He reports consulting for Amgen and Glenmark and travel payments from Eli Lilly.
- Alexander reports consulting and/or honorarium from AbbVie, Akros, Antev, AtriCure, Bayer, Bristol-Myers Squibb, CryoLife Inc, Ferring, GlaxoSmithKline, Janssen Pharmaceuticals, Novostia, Pfizer, Portola, Quantum Genomics, and Veralox.





Comments