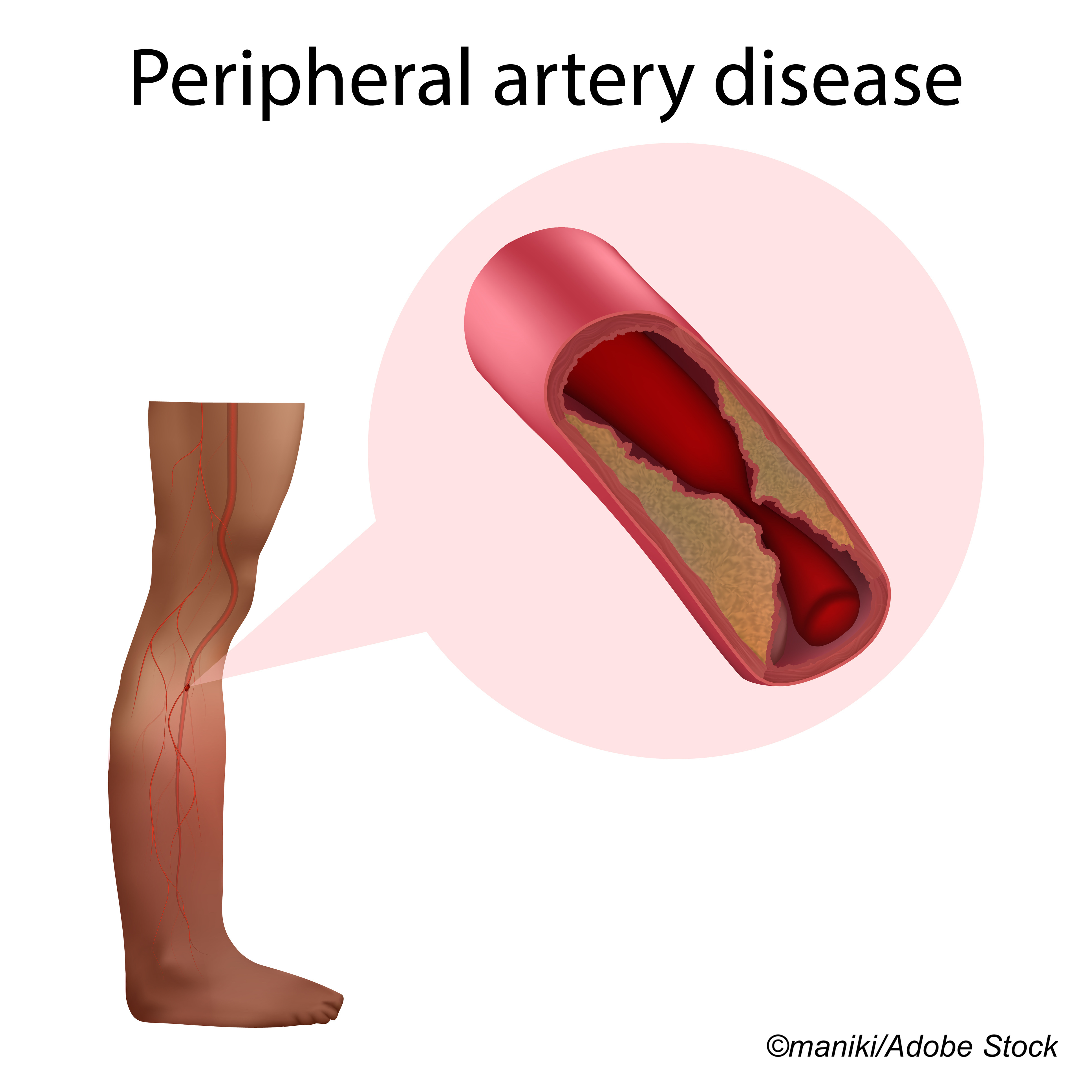
The use of statin therapy in patients with peripheral artery disease (PAD) undergoing peripheral revascularization is not as high as it should be, despite evidence of its benefits, according to results from a retrospective, cross-sectional study published in JAMA Network Open. In fact, researchers found that a full one-fourth of these patients were not on any statin therapy at the time of revascularization, and after revascularization, only 30% were newly prescribed statins.
“The use of antiplatelet and statin therapy in individuals with lower extremity (LE) peripheral artery disease (PAD) for the prevention of cardiovascular morbidity and mortality is well established and endorsed in current clinical practice guidelines. Statin therapy is associated with a reduction in major vascular events, symptom progression, and the need for peripheral revascularization. Statin therapy reduces all-cause mortality and adverse limb events in patients with LE PAD. Despite these benefits and the recommendation for their use, statin therapy in patients with PAD remains suboptimal, even in those whose PAD has progressed to the point of requiring revascularization,” wrote Nikhil Singh, MD, of The University of Chicago, and fellow researchers.
In this retrospective cross-sectional study, Singh and colleagues used data from the Vascular Quality Initiative registry to identify 125,791 patients (mean age: 67.7 years; 62.7% male; 78.7% White) who underwent revascularization between 2014 and 2019 for lower extremity PAD in whom statin therapy was indicated, and with available preprocedural and postprocedural statin data.
The analysis showed improvement in the overall rates of statin prescribing at discharge, from 75% in 2014 to 87% in 2019. Researchers still found, however, that only 30% of these patients not already prescribed statin therapy at the time of revascularization were newly discharged with a prescription for statin medication.
After endovascular intervention, new statin prescription rates were significantly lower compared with after lower extremity bypass (26% versus 41%, respectively).
An increased likelihood of a new statin prescription was associated with the presence of the following characteristics:
- Body mass index ≥30 (OR: 1.13; 95% CI: 1.04-1.24; P˂0.001).
- Diabetes (OR: 1.22; 95% CI: 1.05-1.41; P=0.01).
- Smoking (current vs never: OR: 1.32; 95% CI: 1.21-1.45; P˂0.001).
- Hypertension (OR: 1.19; 95% CI: 1.09-1.29; P˂0.001).
- Coronary heart disease (OR: 1.26; 95% CI: 1.17-1.35; P˂0.001).
In both the endovascular intervention and lower extremity bypass groups, a decreased likelihood of a new statin prescription was associated with female sex, older age, use of antiplatelets, and previous peripheral revascularization.
In their accompanying editorial, E. Hope Weissler, MD, and W. Schuyler Jones, MD, both of Duke University School of Medicine, Durham, North Carolina, reviewed the discrepancies in statin prescribing in patients with PAD.
“Statin prescriptions are the subject of perennial focus among peripheral artery disease (PAD) clinicians and researchers because of the tension between the robust evidence showing that statins significantly improve outcomes and the substantial literature showing that statins are markedly under prescribed. The shortfall in statin prescriptions is an especially pressing matter in the study and treatment of PAD because of the sheer burden of cardiovascular and limb events affecting patients with PAD, which appropriate statin therapy has been estimated to reduce by 25% (for mortality) to 33% (for amputation). Given 57,000 annual deaths and 148,000 annual major amputations among patients with PAD in the United States, of whom 6% to 18% are estimated to be taking statins of appropriate intensity, the scope of the opportunity is clear,” they wrote.
They stressed that an important limitation in this study is the lack of data on variations between institutions in conversion to statin prescribing.
Other study limitations listed by Singh et al include the failure to assess and quantify adverse cardiac or limb outcomes according to new statin discharge prescription status, possible errors in excluding patients not receiving statin therapy, lack of data on statin therapy intensity, and the low ratio of endovascular to surgical interventions.
“Whether statin under prescription is associated with lack of knowledge, lack of initiative, or lack of consequences, it is clear that current quality incentives alone are insufficient. It may be necessary to link statin prescription more explicitly with procedural reimbursement, in recognition of the fact that revascularization events are moments of obligate contact between patients with PAD and PAD experts. An argument could be made that clinicians who are not enough aware of PAD guidelines to prescribe statins appropriately may also merit greater scrutiny of their other PAD-related decision-making (ie, revascularizations). At the same time, as the PAD experts, revascularizing clinicians need to proactively engage primary care clinicians and patients as colleagues to understand barriers to statin prescription (and persistence) at a local level,” wrote Weissler and Jones.
“While the reasons behind under prescription of statins are academically interesting and important to understand, ongoing collective failure to begin enacting solutions to improve prescription of guideline-directed PAD therapies has real world consequences for the hearts, limbs, and lives of patients,” they concluded.
-
Only 30% of peripheral artery disease (PAD) patients undergoing peripheral revascularization who were not receiving statin therapy at the time of revascularization were discharged with a new statin prescription.
-
New statin prescriptions were especially low in PAD patients after endovascular intervention.
Liz Meszaros, Deputy Managing Editor, BreakingMED™
Singh reported no disclosures.
Weissler and Jones reported no conflicts of interest.
Cat ID: 206
Topic ID: 74,206,730,206,192,925,159


